Nanoparticles
The next frontier of medicine
Researchers are using nanoparticles to target drugs at specific cells, like cancer, avoiding the harmful side effects these treatments have on the rest of the body.
Warning: This story contains potentially distressing content about preterm birth.
Therapies for cancer and preterm labour are two examples of drugs which have their desired effect, but can also have devastating outcomes for overall health.
This is because the drugs involved spread throughout the body rather than being targeted to a specific site.
Researchers are solving this problem with nanoparticles.
While nanoparticles are defined as being between one and 100 nanometres (nm) in diameter – roughly 1000 times smaller than a human hair – particles up to 500nm are sometimes included.
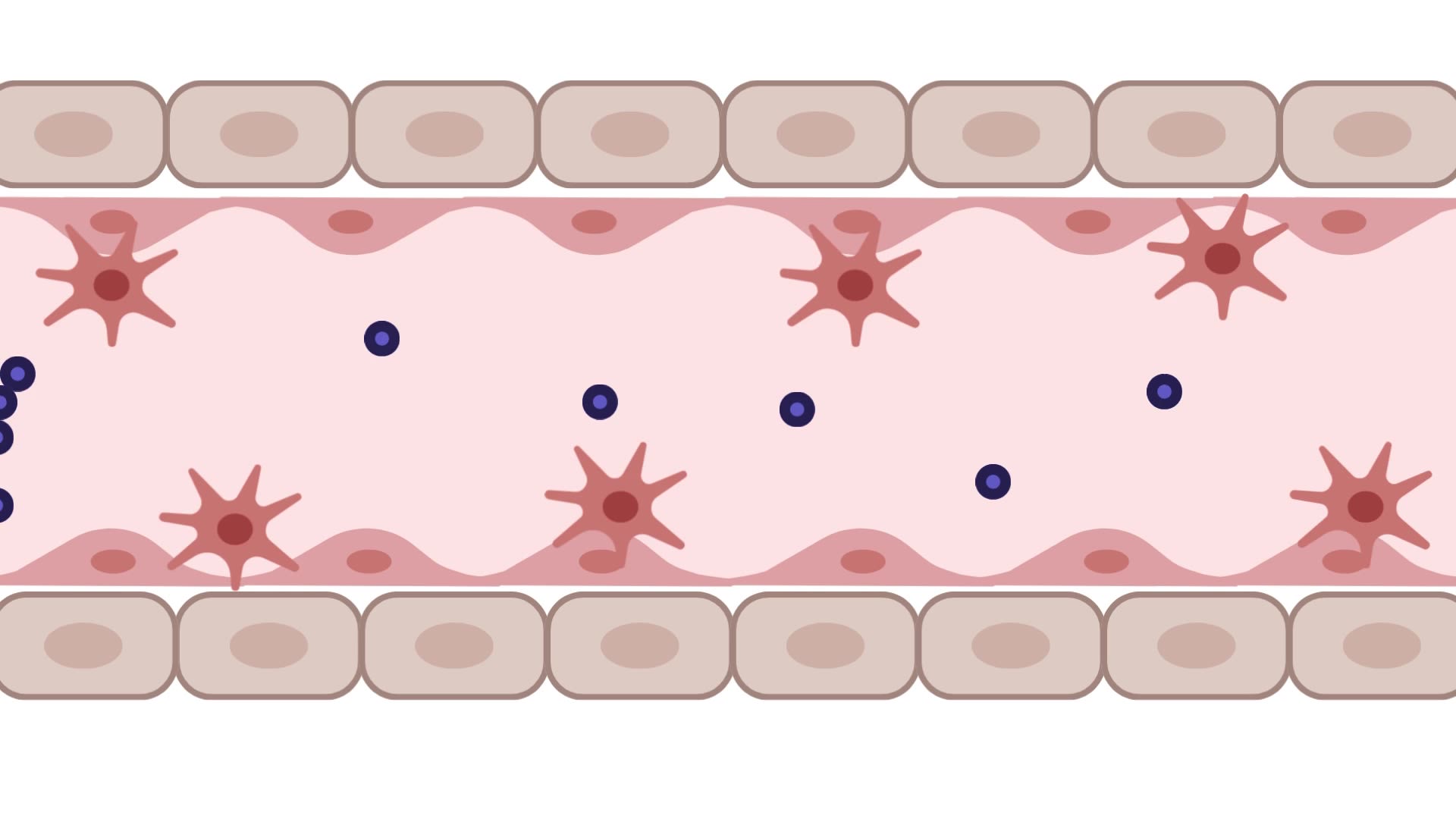
This means nanoparticles can reach places larger molecules, like red blood cells, cannot. Similar to a Trojan Horse, the particles are loaded with cargo - in this case drugs - which they then to delivery to specific sites.
Therapies for cancer and preterm labour are two examples of drugs which have their desired effect, but can also have devastating outcomes for overall health.
This is because the drugs involved spread throughout the body rather than being targeted to a specific site.
Researchers are solving this problem with nanoparticles.
While nanoparticles are defined as being between one and 100 nanometres (nm) in diameter – roughly 1000 times smaller than a human hair – particles up to 500nm are sometimes included.
This means nanoparticles can reach places larger molecules, like red blood cells, cannot. Similar to a Trojan Horse, the particles are loaded with cargo - in this case drugs - which they then to delivery to specific sites.
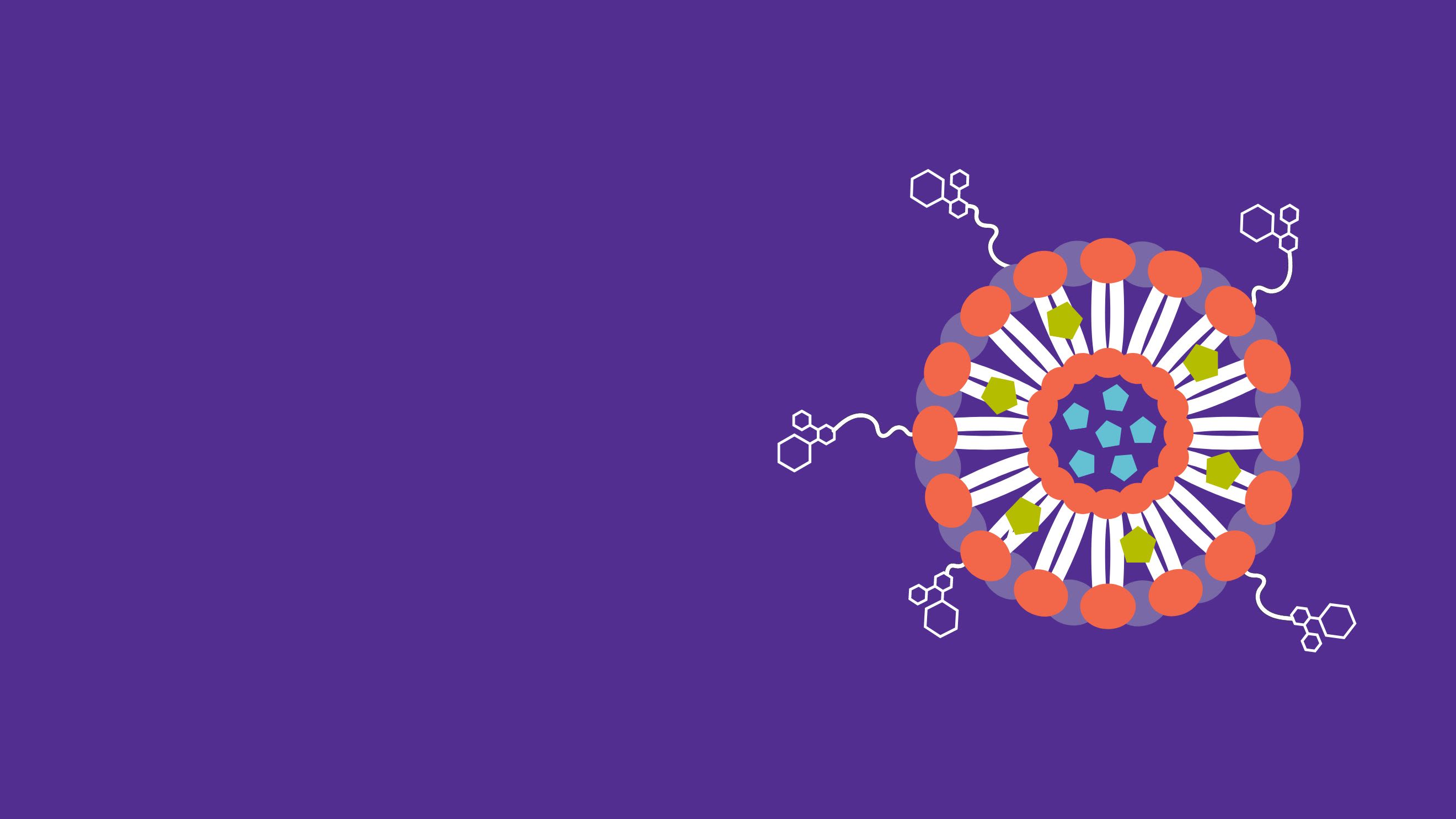
There are a range of nanoparticle types which can be both organic or inorganic.
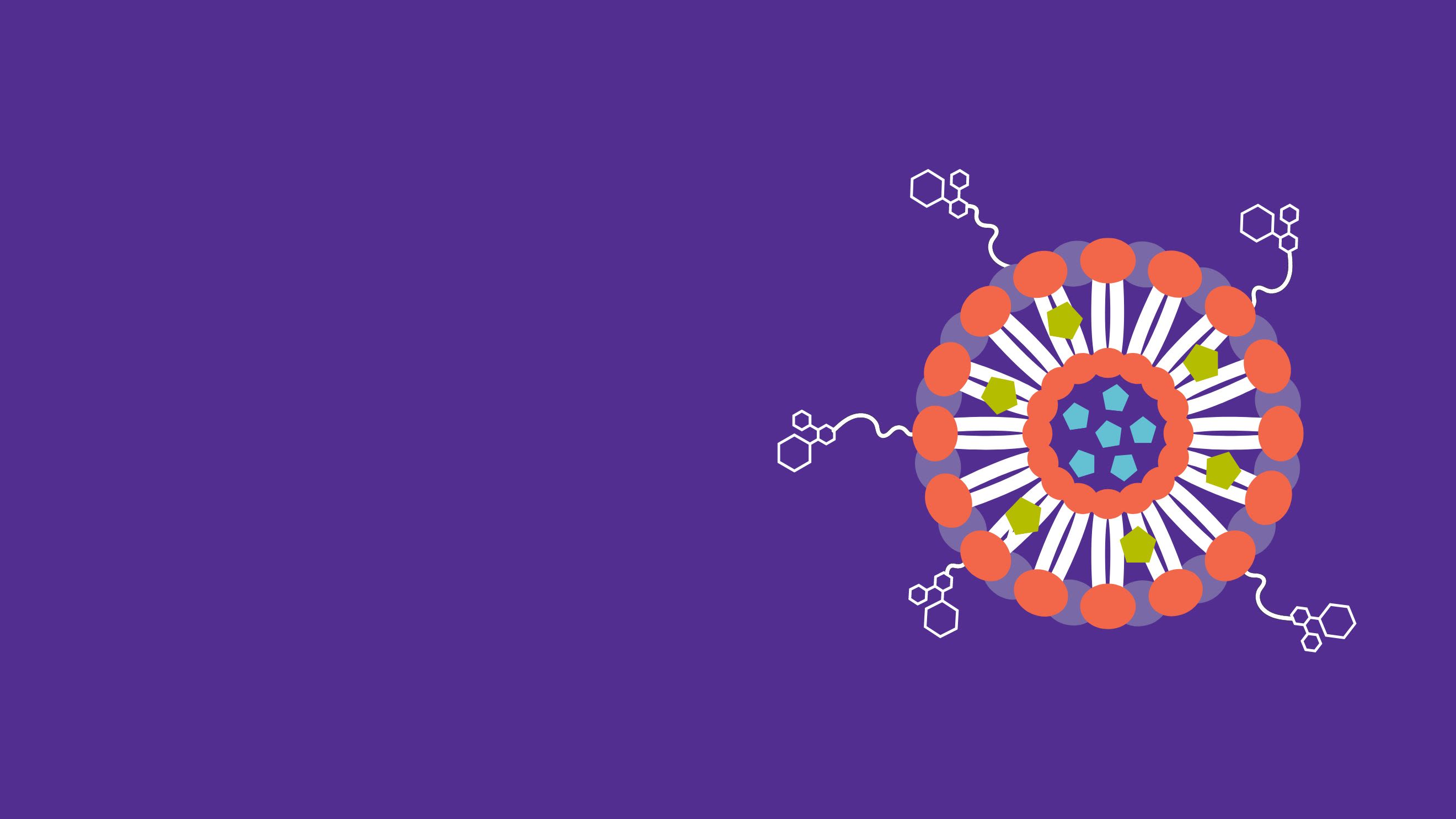
The Hunter Medical Research Institute (HMRI) Mothers and Babies Research Program works with organic nanoparticles called nanoliposomes, which consist of fat molecules like those in human cells.
The fat molecules are arranged in a sphere around a water core. This gives nanoliposomes the ability to carry both fat-soluble and water-soluble drugs. When drugs are loaded into the nanoliposomes prior to being administered, they are protected from degradation in the bloodstream and risks of drug toxicity and side effects are reduced.
The team are now working on ways to target these nanoliposomes, and the drugs they carry, to specific sites within the body - a concept pioneered at HMRI by Mothers and Babies Scientific Director Distinguished Laureate Professor Roger Smith AM.
Roger works closely with Program Co-Director Dr Jonathan Paul and researcher Dr Jorge Tolosa, who are leading nanoparticle work in the areas of premature birth and ovarian cancer, respectively.
Preventing
preterm birth
In 2022, Bryanna Budge was one of the almost one million mothers who lost their babies to premature birth.
“At 18 weeks we announced our pregnancy on social media,” Bryanna says.
“And then the next day at 11 o’clock my waters broke. I was told that afternoon that my baby would be here before we knew it.”
During a night of intense labour, Bryanna says she tried to come to terms with what was happening and prayed that the pregnancy wouldn’t have to end.
“They came in to check the next morning and I asked if there was anything I could do just to keep it a little longer. But they said it was too late.”
That day, in the shower, Bryanna miscarried her first daughter at a little more than 18 weeks.
“I didn’t want to let her go. Just holding on to her and as tiny and fragile as she was saying ‘Just breathe, you’re going to be here with me’.”
Bryanna describes the emotional trauma of preterm birth and the difficulty of having to "say goodbye". The following day, she left the hospital carrying a box instead of her newborn baby.
“That was very difficult and something I never thought I would have to go through,” she says.
“Seeing other mums and pregnant women walking past me as I was just leaving with a box.”
Thankfully Bryanna and her partner have since welcomed a healthy baby girl into the world.
But their story of loss is all too common and there is currently no way of effectively stopping premature labour once it has begun.
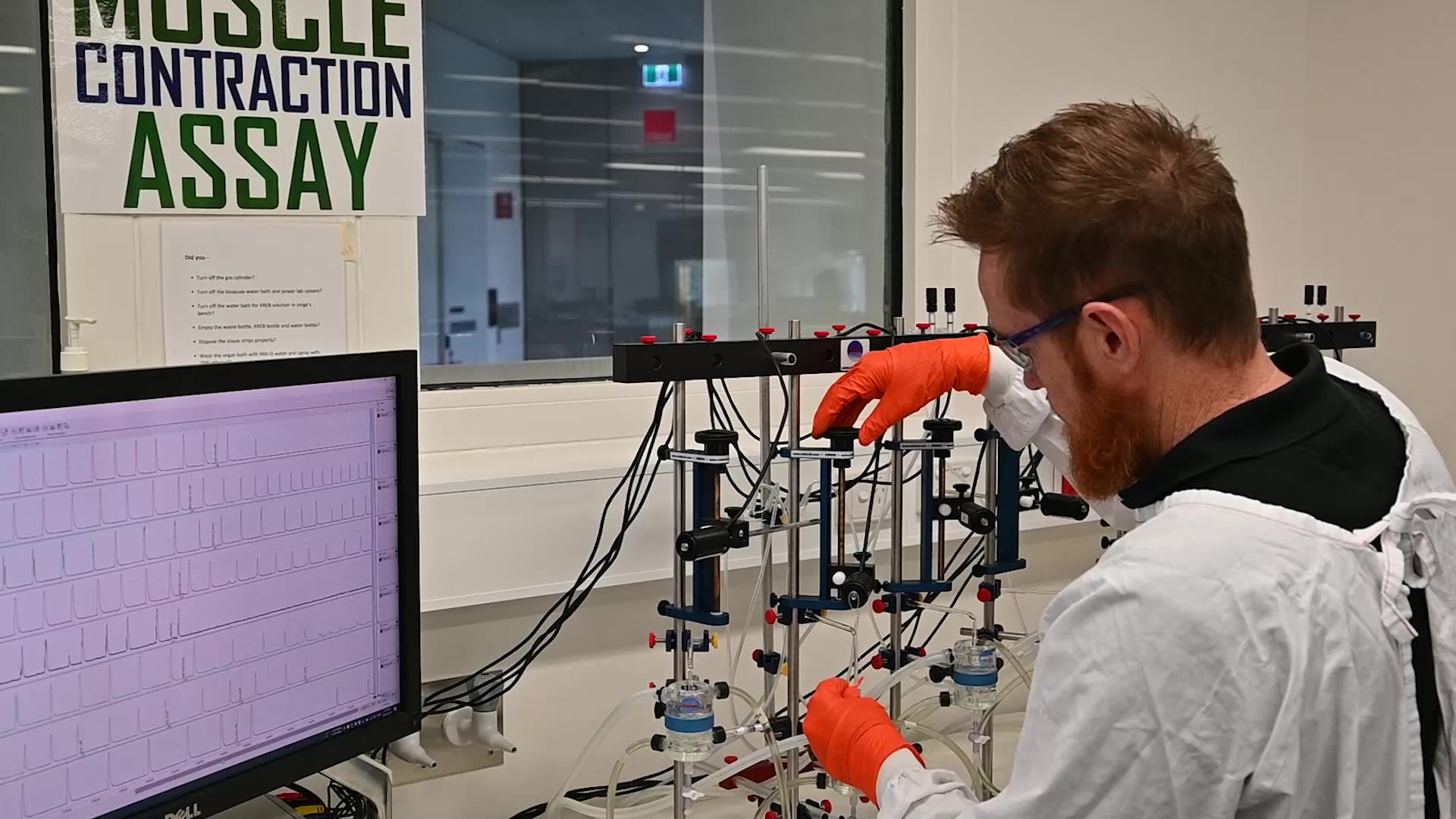
Having identified new drug combinations to stop preterm labour contractions, Dr Jonathan Paul is working on ways to deliver these drugs specifically to the uterus.
This targeted drug delivery is significant because current treatments for preterm labour work by slowing down muscle contractions and often target smooth-muscle cells, like those of the uterus.
The problem is that uterine smooth muscles share a lot of similarities with other smooth muscle tissues, such as blood vessels and the heart, where slowing down contractions can have serious consequences.
“When drugs are administered to block preterm labour they can affect other organs and tissues causing side effects that can place the mother's health at serious risk,” Dr Jonathan Paul says.
"These drugs may also cross the placenta. Producing side effects in the baby."

During pregnancy, uterus cells have increased
levels of the receptor for the hormone oxytocin.
To take advantage of this, Jonathan and his team
have coated nanoparticles in antibodies and peptides
that specifically bind to the oxytocin receptors.
“Our targeted nanoparticles increase the proportion
of drug cargo that reaches the pregnant uterus,” Jonathan says.
“While simultaneously reducing the amount of drug cargo
that goes to non-target organs where it causes side effects.”

During pregnancy, uterus cells have increased levels of the receptor for the hormone oxytocin.
To take advantage of this, Jonathan and his team have coated nanoparticles in antibodies and peptides that specifically bind to the oxytocin receptors.
“Our targeted nanoparticles increase the proportion of drug cargo that reaches the pregnant uterus,” Jonathan says.
“While simultaneously reducing the amount of drug cargo that goes to non-target organs where it causes side effects.”
During pregnancy, blood vessels around the uterus develop small holes known as fenestrations
Nanoparticles are small enough to exit the blood vessels in which they are being carried – through the fenestrations - into the space around smooth muscle cells of the uterus.
Here they have direct access to bind to oxytocin receptors.
“Using nanoparticles to achieve uterine-targeted delivery has broadened the therapeutic approaches we can explore for safely and effectively preventing preterm birth," Jonathan says.
HMRI Mothers and Babies researchers have been exploring the medical uses for nanoparticles beyond preterm birth.
Treating
ovarian cancer
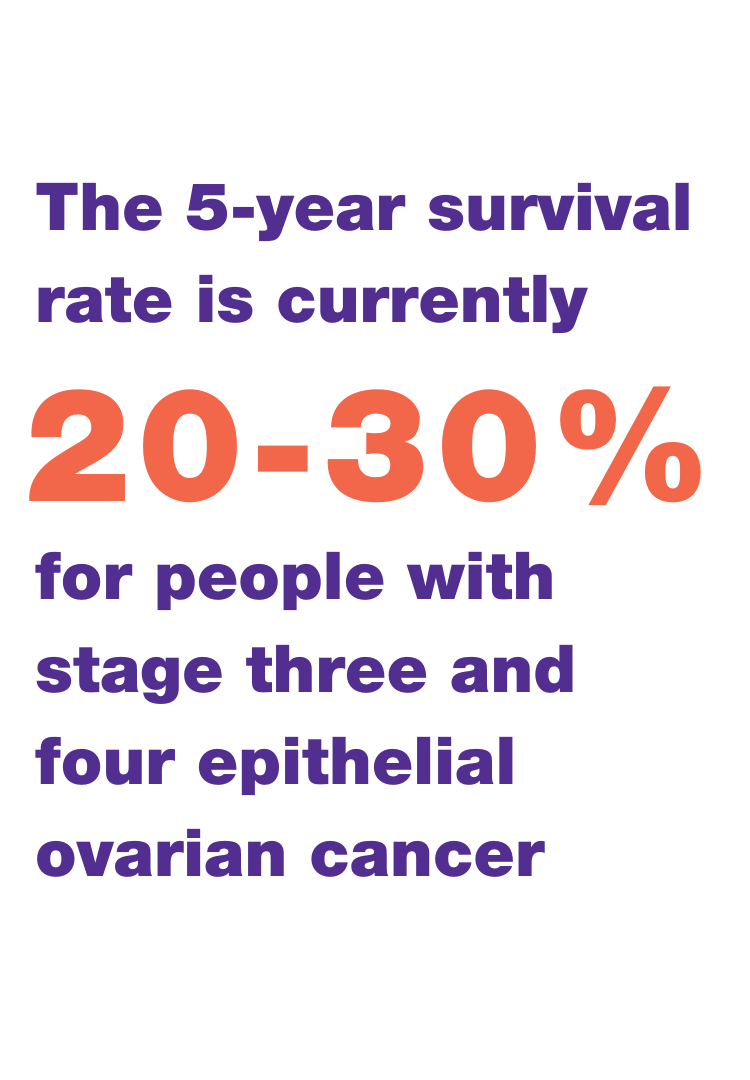
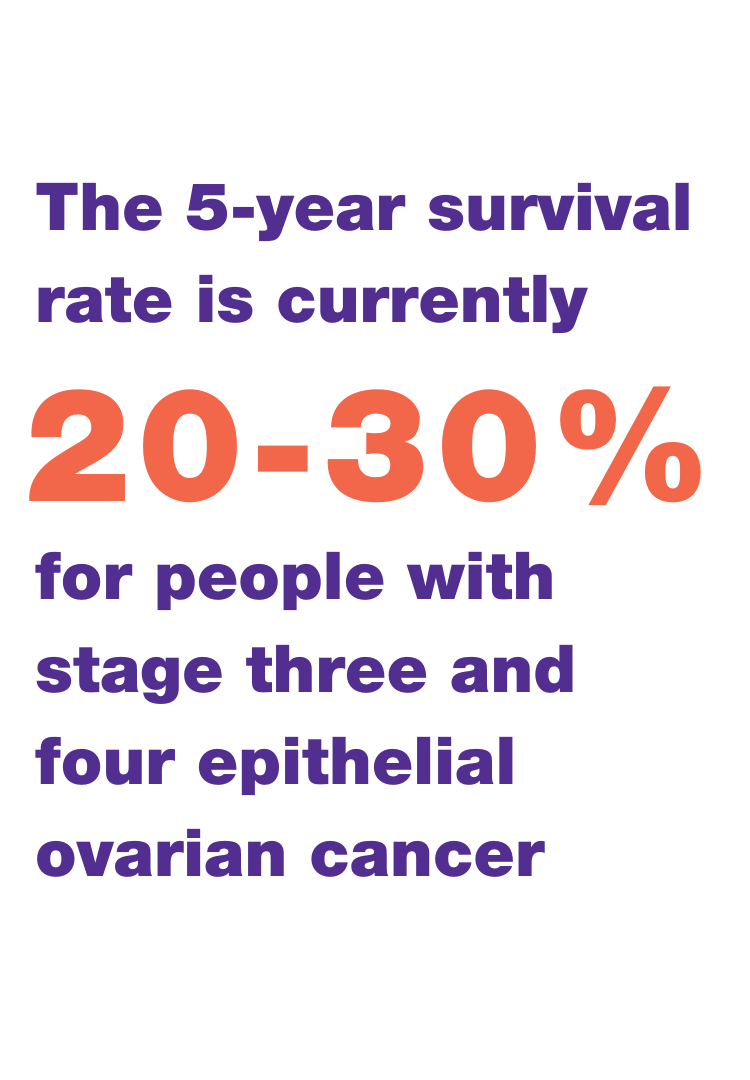
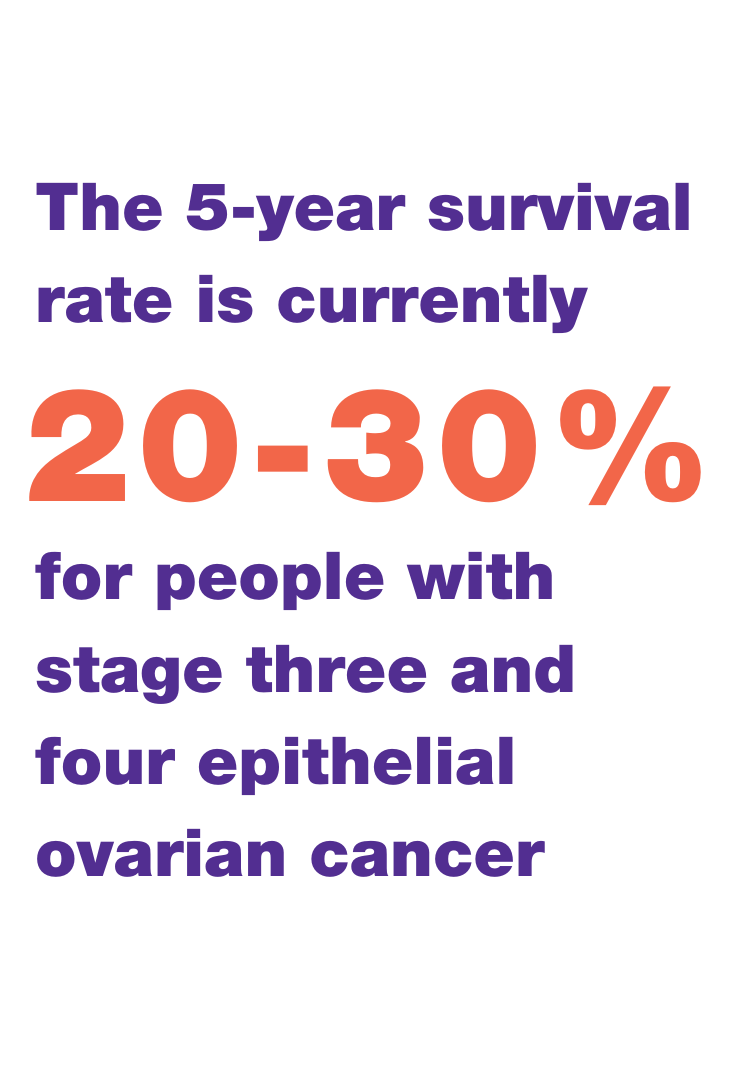
There were more than 1100 ovarian cancer related deaths in Australia during 2023, with the current five-year survivorship around 50%.



Mothers and Babies Research Program founder, Roger Smith, describes ovarian cancer as one of the most challenging cancers to manage.
“Ovarian cancer is the leading cause of cancer amongst gynaecological malignancies worldwide,” Roger says.
About 90% of ovarian cancer cases are described as being epithelial and arise from cells outside the ovary.
Less than 30% of women with stage three and four epithelial ovarian cancer survive to five years after diagnosis.
When individuals are diagnosed with cancer, treatment usually involves surgery coupled with chemotherapy, radiation or sometimes both.
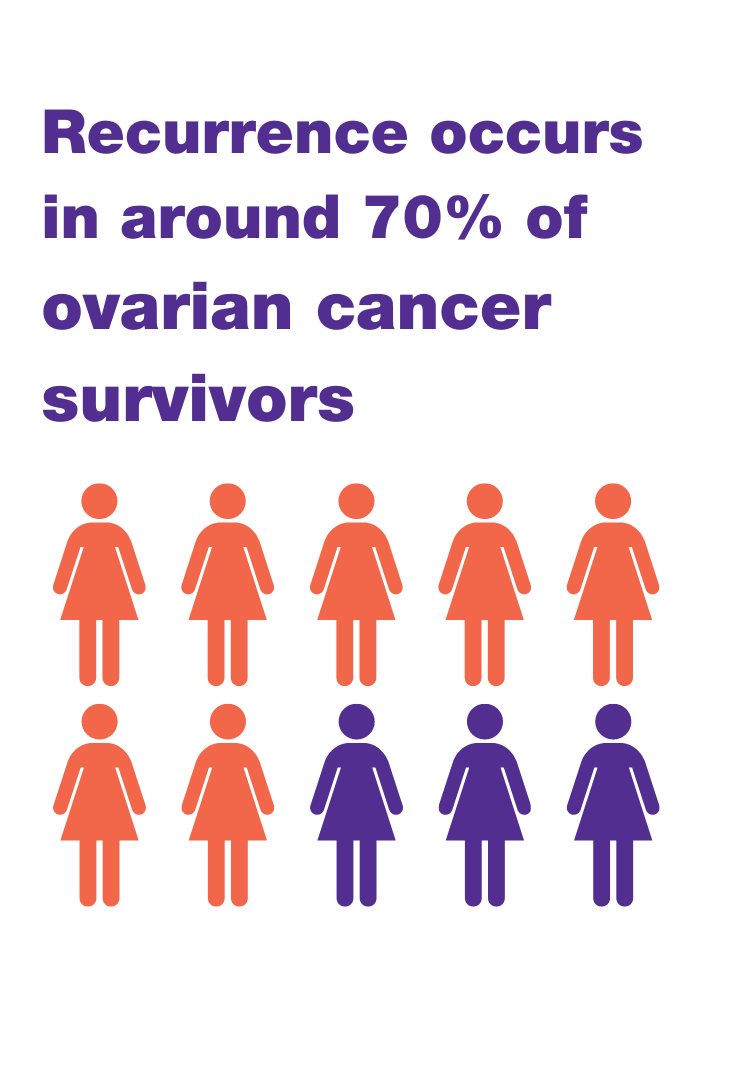
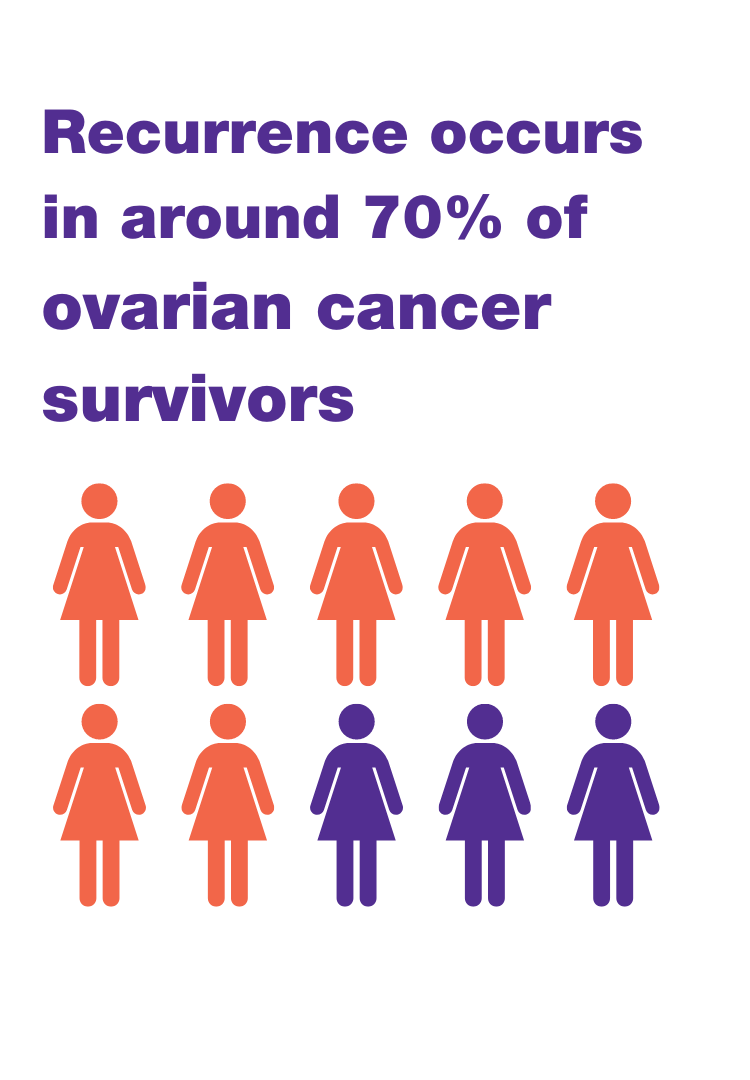
“Unfortunately, remission is generally short-lived and cancer recurs in at least 70% of patients.”
The drugs used can also have devastating impacts on a patient’s overall health.
Because of this, Roger and his team are working on ways to use nanoparticles for more effective and targeted treatment of ovarian cancer.
Mothers and Babies Research Program founder, Distinguished Laureate Professor Roger Smith AM, describes ovarian cancer as one of the most challenging cancers to manage.
“Ovarian cancer is the leading cause of cancer amongst gynaecological malignancies worldwide,” Roger says.

About 90% of ovarian cancer cases are described as being epithelial and arise from cells outside the ovary.
When individuals are diagnosed with cancer, treatment usually involves surgery coupled with chemotherapy, radiation or sometimes both.
The drugs used can also have devastating impacts on a patient’s overall health.
Because of this, Roger and his team are working on ways to use nanoparticles for more effective and targeted treatment of ovarian cancer.
The body’s natural filtration system poses a significant challenge for researchers trying to target nanoparticles to particular cell - such as those of the ovary - with less than 1% of nanoparticles successfully reaching solid tumours.
Part of this problem is that the liver sequesters nanoliposomes - primarily in their Kupffer cells - prior to the particles reaching their destination.
Jonathan says to overcome this issue, his team coats nanoparticles with polyethylene glycol (PEG), to reduce Kupffer cell uptake.
They then incorporates specific ligands to the surface of nanoparticles.
“These ligands allow the nanoliposomes to be targeted to specific cell types within tissues,” Jonathan says.
Leading the program’s work on ovarian cancer are Dr Jorge Tolosa, along with PhD student Ester Barau Dalmau.
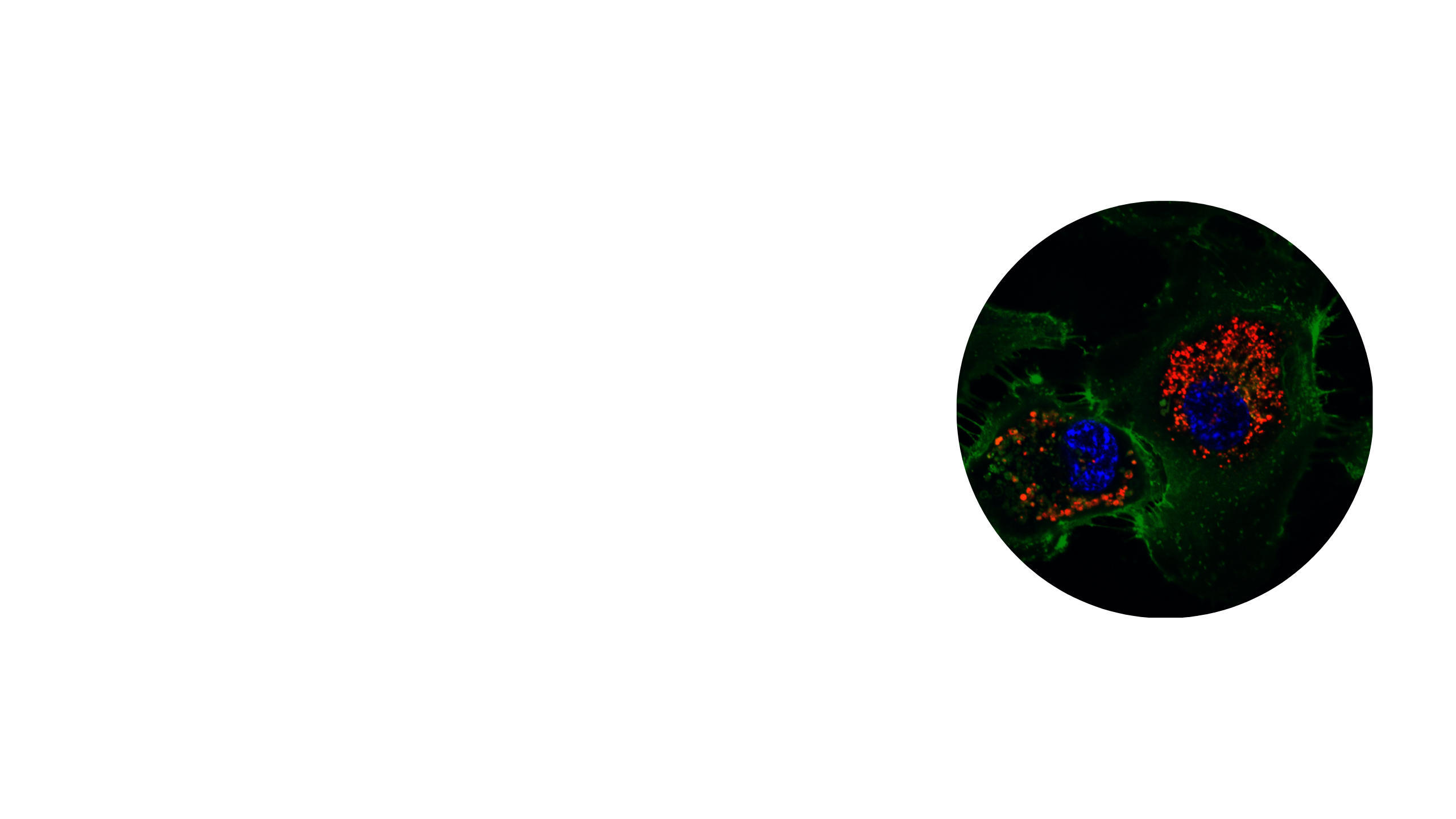
Their research has found that coating nanoparticles in specific peptides significantly increases the delivery of drugs to endothelial and ovarian cancer cells.
The body’s natural filtration system poses a significant challenge for researchers trying to target nanoparticles to particular cell - such as those of the ovary - with less than 1% of nanoparticles successfully reaching solid tumours.
Part of this problem is that the liver sequesters nanoliposomes - primarily in their Kupffer cells - prior to the particles reaching their destination.
Jonathan says to overcome this issue, his team coats nanoparticles with polyethylene glycol (PEG), to reduce Kupffer cell uptake.
They then incorporates specific ligands to the surface of nanoparticles.
“These ligands allow the nanoliposomes to be targeted to specific cell types within tissues,” Jonathan says.
Leading the program’s work on ovarian cancer are Dr Jorge Tolosa, along with PhD student Ester Barau Dalmau.
Their research has found that coating nanoparticles in specific peptides significantly increases the delivery of drugs to endothelial and ovarian cancer cells.
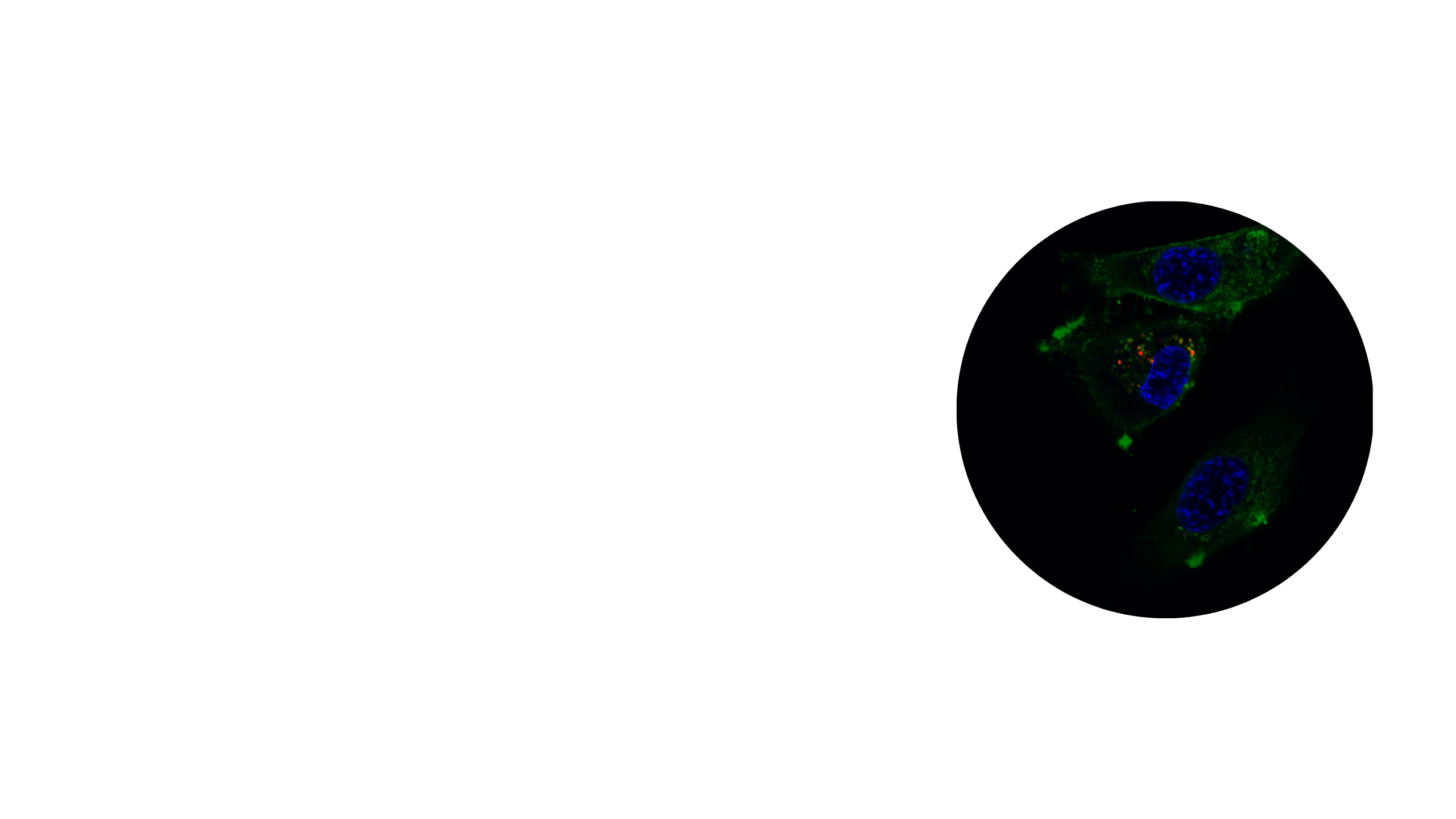
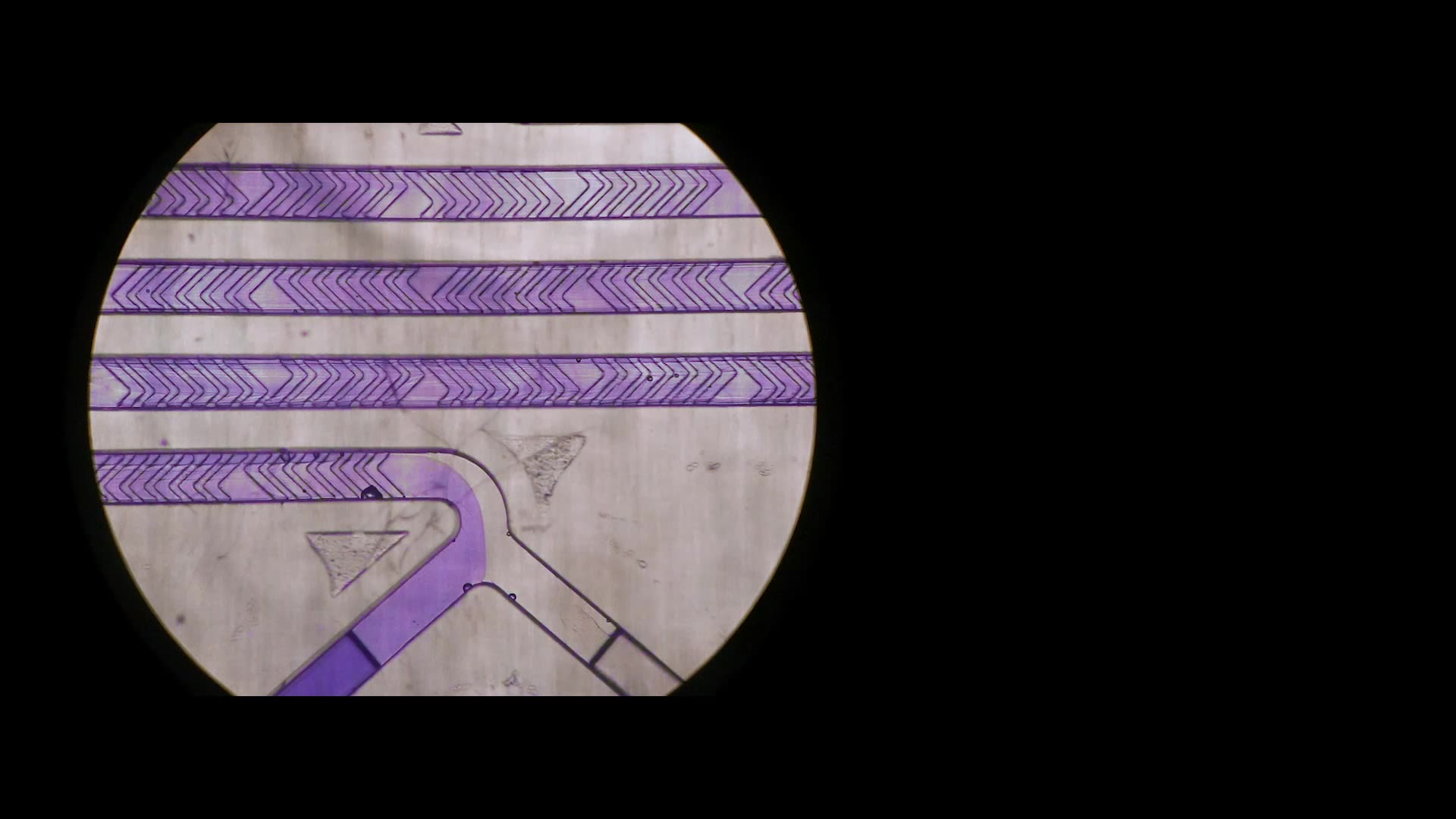
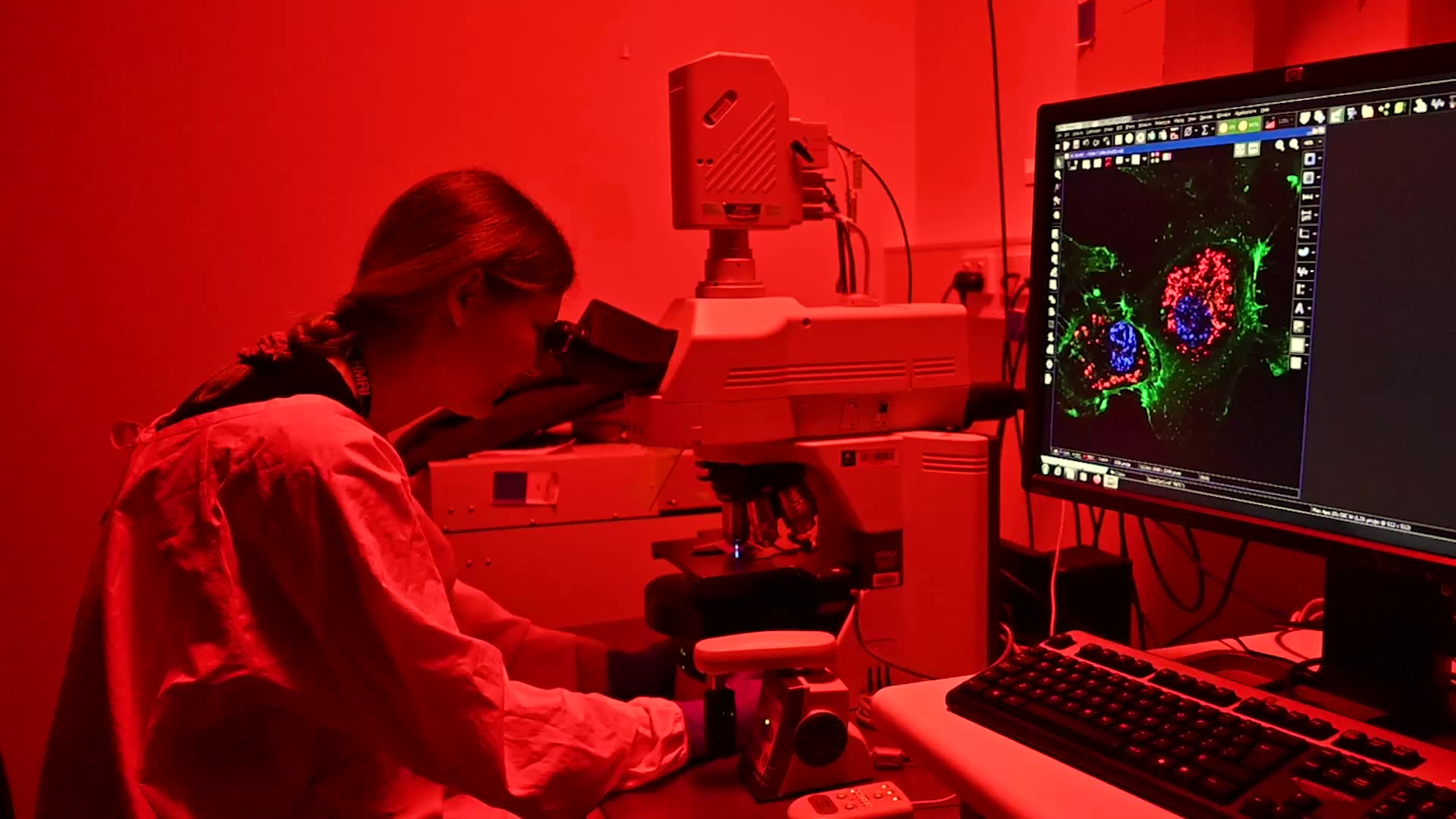
This image, taken under a microscope, shows the nucleus and cytoplasm of endothelial cells after non-targeted nanoparticles have been administered.
This is contrasted with an image of the same area following targeted nanoparticle treatment. It is clear how successful these nanoparticles are in entering the endothelial cell compared with the previous non-targeted image.
They are also exploring ways to block the mononuclear phagocyte system, which includes the liver, in order to deliver more drugs to the target cells.
“Current approved nano-formulations often profoundly improve the safety profile of drugs,” Jorge says.
“However, they do not substantially improve overall cancer patient survival. This is due to inefficient delivery of nanoparticles to tumour sites.”
By blocking this system and coating the nanoparticles in specific peptides, the team has successfully targeted the ovary and reduced nanoparticle uptake in other organs.
“Targeted nanoparticles have the potential to improve therapeutic outcomes in many clinical settings. To achieve this exciting goal, each part of the complex journey the particle takes from delivery of the therapeutic, to action at the target cell, must be optimised.”
Too many lives are lost to ovarian cancer each year, with treatment itself often having devastating health impacts. The HMRI Mothers and Babies Research Program is working on ways to effectively and accurately target hard to treat cancers, using nanoparticles.
These dedicated researches are also developing ways to use the same type of particle to prevent preterm birth, so parents like Bryanna's don't have to endure the loss of a child.
Published date: 08 August 2024